No English 651-431-2000
Need health care coverage?
Minnesota’s public health care programs provide health care coverage to Minnesotans with low to no income. We encourage anyone who needs health care coverage to apply to see if you qualify for Medical Assistance or MinnesotaCare, including those Minnesotans who had work hours reduced, have been furloughed or who have lost their jobs.
Medical Assistance is Minnesota’s Medicaid program. MinnesotaCare is a premium-based program for people who earn too much to qualify for Medical Assistance but make too little to pay for private insurance. Those who qualify for MinnesotaCare never pay more than $80 a month per person for their premium. The programs have income and asset limits that depend on your age, who you live with, and whether you are pregnant, blind or have a disability. They offer comprehensive coverage, including dental benefits and vision and behavioral health services.
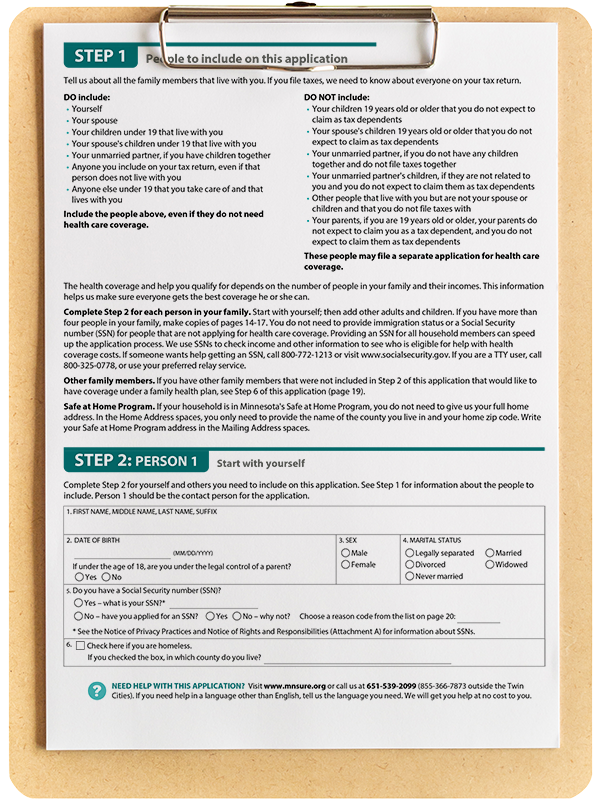
How to apply
Most Minnesotans can apply for these programs online through MNsure, Minnesota's health insurance marketplace. Here are some tips for completing the MNsure online application. Learn more about applying.
Some people should not apply through MNsure. These are typically seniors and people with disabilities:
- If you are 65 or older, please see the page on how to apply if you are a senior.
- If you are have a disability, please see the page on how to apply for people with disabilities.
Need help applying?
Health insurance is complicated stuff. You don’t have to figure it out on your own.
- Connect with a navigator in your community to help you get enrolled. Navigators can help in several different languages. Search the directory for the language easiest for you in which to communicate.
- Call DHS Health Care Consumer Support at 651-297-3862 or 800-657-3672 for help with questions or for a paper application.
- Reach out to your local county or tribal office.
- If you have a disability, contact the Disability Hub MN at 866-333-2466.
- If you’re 65 or older, contact the Senior LinkAge Line at 800-333-2433.
Don’t qualify due to your immigration status?
Emergency Medical Assistance (EMA) provides coverage to undocumented Minnesotans who do not have an immigration status that qualifies for Medical Assistance. EMA covers medical conditions that left untreated within 24-48 hours will:
- Place your health in serious jeopardy.
- Cause serious impairment to your bodily functions.
- Cause serious dysfunction to any of your organs or body parts.
Emergency medical conditions include labor and delivery.
Emergency Medical Assistance may also cover some care and treatment for other conditions and services provided in other settings, including cancer, dialysis, kidney transplants, and care received in nursing homes, psychiatric residential treatment facilities, community settings and homes.
You can apply for Emergency Medical Assistance through your local county or tribal office.
Need help in your own language?
Call the Refugee and Immigrant COVID-19 Help Line to get information on testing locations and related health support.
651-318-0989
Callers can also get help with information on basic needs, distance learning support, employment, financial needs and the process towards citizenship. Help Line staff speak Amharic, Anuak, Arabic, French, Hindi, Karen, Lingala, Luganda, Mashi, Oromo, Somali, Spanish and Swahili. Language line help is available for any other language.
The help line is open from 9 a.m. to 5 p.m. Monday through Friday.
Health care programs are only some of the services you and your family might be eligible to receive. Others may include income assistance, child care, housing and food support.